“I have multiple sclerosis, because I thought why stop at one?”
Tim Ferguson
If you’re anything like me when MS was mentioned as a possible explanation for my symptoms, I was searching my brain to remember what that stood for. None of the doctors or technicians during the investigation stage elaborated on what MS was, it seemed to be a given that everyone knew, including me. Of course, I could have asked what it meant at the time but I was in a cold sterile room hearing some serious news, that I would need full body MRIs for a definitive diagnosis and they would organise those for me as soon as possible. I was swamped. There is nothing like a concerned doctor pulling strings to get you into a packed MRI facility for a scan immediately that makes your heart race and your brain not focus on little things, like what MS stood for. After all, everyone else seemed to know, I didn’t want to sound ignorant. It sounded familiar and I vaguely remembered fundraising events when I was at school. All I knew for sure was it’s serious, so I figured I would look it up later.
What is MS
- Disease action in multiple sclerosis
- Types of MS
- Potential symptoms
- Diagnosis
- Treatment options
- Where to next
Disease action in multiple sclerosis
Multiple sclerosis is a disease of the central nervous system that interferes with the nerve impulses of the brain, spinal cord, and optic nerves. It is a demyelinating disease whereby the insulating covers of the nerve cells (neurons) in the brain and spinal cord are damaged, disrupting the transmission of nervous systems signals. This damage is caused in part by our own immune system, mistakenly identifying our own neurons as foreign and attacking them. Ordinarily our immune system, specifically our T cells, are prevented from entering our brains through the protection of our blood-brain barrier, however in people with MS this barrier is disrupted allowing T cells to enter and damage our central nervous system. This results in the development of lesions, a kind of scarring, and inflammation. Depending on where these lesions develop it will manifest into various symptoms, no two people are impacted the same way by multiple sclerosis.
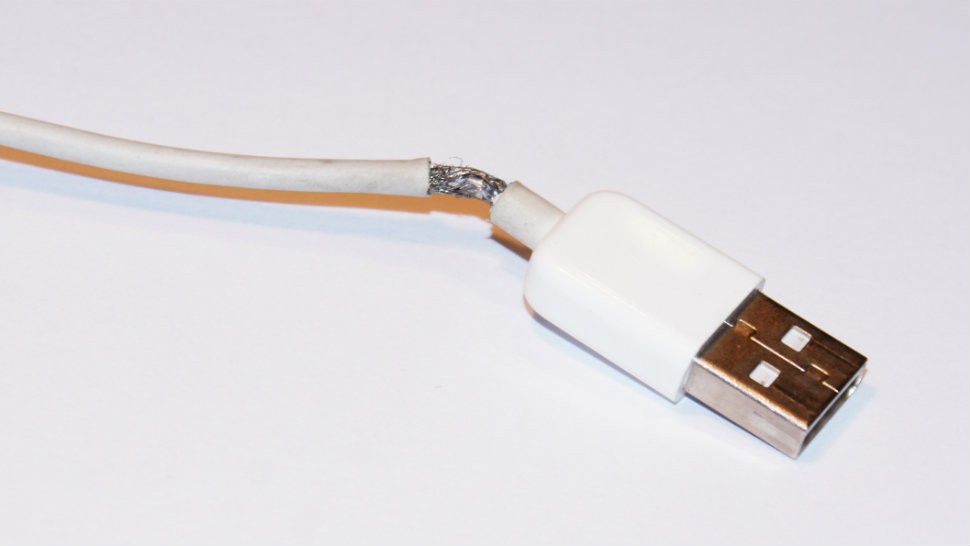
Picture a charging cable for your phone. On the outside is a protective plastic sheath that houses the wires which transmit electricity from the plug to your phone. Have you ever had one of those cables become a bit dodgy? The plastic sheath has started coming away, and the wires inside have started to fray? How well does your phone charge with a cable like this? This is a broad analogy of what the action of demyelination is like. The neurons without our brains have axons which are like those charger cables transmitting the electrical signals of our brains around our bodies. These axons are protected by myelin sheath, like the protective plastic sheath around our charger cables. In multiple sclerosis the myelin sheath becomes damaged and just like a dodgy charger cable missing some of the protective plastic sheath doesn’t work well anymore, the axon missing some protective myelin sheath has trouble transmitting the signals around the body.

A frayed cable can no longer charge your phone or transfer data as efficiently as it once did.
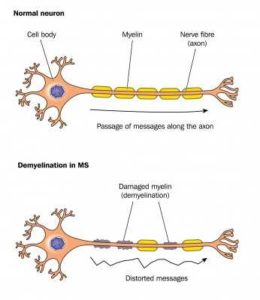
During active relapses our bodies immune system damages the protective myelin sheath. Our neurons no longer transmit information as effectively.
There is no known cause of multiple sclerosis, but it is believed that it is triggered by a suite of environmental factors in individuals with complex genetic-risk profiles. For more detailed information on the pathophysiology of multiple sclerosis see the Wikipedia page. This page is updated fairly regularly and so is a good first stop for information.
Types of multiple sclerosis
There are four main types of multiple sclerosis;
- Clinically isolated syndrome
CIS is often what people are diagnosed with first before a concrete diagnosis of RRMS. A person with CIS has had an attack suggestive of a demyelination event but it does not yet meet the criteria for a definitive diagnosis of multiple sclerosis. Many people, but not all, who are diagnosed with CIS will go on to later develop MS.
- Relapsing remitting MS
RRMS is characterised by unpredictable relapses followed by periods of no new signs of disease activity that can last months or years. This is known as remission. A relapse is when damage is occurring to your central nervous system and new lesions are forming, however not all lesions occur somewhere that presents a physical or measurable impact, i.e. there is the potential for silent lesions contributing to your overall disease burden. After each relapse there is the potential to return to your full functionality as before, or you will retain some of the impacts of that relapse, adding to your overall disability. Whilst you are likely to become more disabled over time, and to need some kind of walking aid (i.e. a walking stick or wheelchair) later in life, it is not something to be disheartened by. You may have long periods of remission allowing you to live a fulfilling life and preparing yourself so you are able to adapt to any changes after your next relapse.
- Primary progressive MS
PPMS occurs in 10-20% of individuals and is characterised by no periods of remission after the initial symptoms, that is the progression of disability as the lesion load increases with no or only minor improvements after each relapse.
- Secondary progressive MS
SPMS occurs in 65% of people with RRMS who progress to increasing neurologic decline between relapses without any periods of remission, that is the gradual worsening of function and increase in disability with little to no improvements over time.
I was diagnosed with CIS but due to the extent of damage found in my spine and on my brain, as well as the presence of protein bands in my lumbar puncture the diagnosis was formalised to relapsing-remitting multiple sclerosis. As my experience is with RRMS this is the focus of my content, though for those of you with the other forms of multiple sclerosis, I truly hope my website provides something useful for you, even if it’s a place to start from.
What is important to remember is that your multiple sclerosis may change and evolve over time, your experience of multiple sclerosis will be unique to you…
What is important to remember is that your multiple sclerosis may change and evolve over time, your experience of multiple sclerosis will be unique to you, so if you arm yourself with knowledge of what is happening to you and what you can control to help cope with the changes you put yourself in the best position to maintain a healthy and fulfilling life.
Potential symptoms of multiple sclerosis
The symptoms of multiple sclerosis are unique to every individual and depending on the location and severity of your lesion it can impact almost any part of your visual, motor, sensory or autonomic systems. They may develop all at once, or what I suspect has happened to me is that the symptoms have been so mild initially that I dismissed them until they became something I couldn’t ignore. Some (but not all) of the most common early symptoms include:
- Unexplained muscle weakness, loss of sensitivity or numbness, or changes in sensations such as tingling, or pins-and-needles in the arms, legs, or one side of your face.
- Loss of balance, vertigo, difficulty in moving or coordination.
- Blurred vision, double vision or partial vision loss – optic neuritis is a common initial symptom reported in MS
- Loss of functions such as difficulty swallowing or speaking, bladder and bowel difficulties
These symptoms may right themselves in a day or a couple of weeks, potentially misleading you into thinking that you have recovered from whatever was wrong without seeking medical attention. You may think some of it is normal, that other people get pins-and-needles in their arms or legs as well but nobody talks about it.
Diagnosis of Multiple Sclerosis
… you may undertake a number of tests whose results together point to a diagnosis of multiple sclerosis.
Your journey through diagnosis starts with the self-reporting of your symptoms to your GP. They may then ask you to do some basic tasks; walk in a straight line, stand on one leg, hold your arms or legs up whilst they push down against them, read an eye chart. They will ask a suite of questions which may include whether MS is in your family. After this, you may be sent for MRI scans, blood tests, visual evoked potentials testing, and/or a lumbar puncture. There is currently no single test that can provide a definitive diagnosis of the disease, instead you may undertake a number of tests whose results together point to a diagnosis of multiple sclerosis.
- MRI scans – of the brain and spine can show the areas of demyelination. A metallic solution containing Gadolinium can be injected as a contrast agent to highlight differences between normal and abnormal tissues. For people with MS it will show areas of active lesions and the existence of inactive lesions, i.e. past lesion events that you may or may not be aware of. You can get an MRI scan of the brain alone, or the brain and spinal cord, the latter taking longer to complete of course than the brain alone.
- Lumbar puncture – this can be used to look for evidence of chronic inflammation in the central nervous system and rule out other infectious diseases that may be causing similar symptoms. If these markers are found in the cerebrospinal fluid but not in your blood it is entirely likely then to reflect inflammation related to damage of your central nervous system rather than inflammation due to damage elsewhere in your body as shown by inflammation markers present in your blood. Specifically, they will look for the presence of oligoclonal bands, inflammation markers found in 75-85% of people with MS.
- Blood tests – to eliminate other conditions with similar symptoms such as Lupus, vitamin or mineral deficiencies, other bacteria or viral infections.
- Visual and sensory evoked potentials test – because of the potential demyelinating damage to the optic nerve and sensory nerves, the nervous system may respond less actively to simulation. Doctors are able to test these pathways and record the activity of your brain to help add weight to an MS diagnosis.
Treatment options for Multiple Sclerosis
There is currently no cure for multiple sclerosis, but there are a multitude of treatment options. I don’t speak of these to promote one over another, but to help you arm yourself with an understanding of your options, of what you should consider, and the questions you can ask your neurologist to ensure you are given the best option for your condition. Treatments are usually through disease-modifying therapies which are designed to slow the progression of the disease and to lower your relapse rate, or easing the specific symptoms a person may have through symptomatic therapies. The disease-modifying therapies act on the immune system, changing the activity of your immune system to slow the frequency and severity of attacks to your central nervous system, meaning less damage to your myelin sheaths. Symptomatic therapies may include steroids which can ease the inflammation at a site of disease activity to reduce the severity of a relapse.
You don’t die of MS, you die with MS.
It is important to talk with your neurologist and to determine what treatment is best for you. My first neurologist assumed I knew what MS was and the treatment I should take, we didn’t discuss side effects, other potential options, or how it would impact my lifestyle. I felt bamboozled and somewhat dismissed, as if I’d gone in complaining of a headache and my doctor gave me a script for paracetamol. Every person will have a different response to different medications and may experience different side effects so it is essential you are and feel informed when you make your choice. There are also your personal circumstances to take into consideration and that you should raise when planning your treatment with your neurologist;
- Family planning – some drugs are safe during pregnancy, others must be out of your system before you fall pregnant;
- Other medical conditions – there are potential interactions between drugs that your neurologist would be able to help you with;
- Employment – some treatments suppress your immune system which may not be a wise choice if you work in an environment that potentially exposes you to a high rate of transmissible diseases or infections, such as working in a day care (kids get sick with things all the time), as a flight attendant, in a hospital etc;
- Travel – infusions require you to attend an out-clinic on a regular basis to maintain the effectiveness of your therapy, or you may have to take more tablets out of country with you with a letter from your neurologist to prove your tablets are real and legal.
Thankfully there are a range of options that you can work through under the guidance of your neurologist to find one that suits you best and will help you to maintain a healthy and fulfilling life.
This factsheet from the MS Australia website has a nicely summarised table to allow you to quickly compare different treatments. They are also a good source of information for all aspects of MS so are a good resource for you moving forward.
Aside from medical based therapies you will easily find yourself overwhelmed with blogs and reports of the best lifestyle and dietary choices for people with MS. To date there is no medical consensus on the best diet, but there are lots of studies showing the benefits and harms of various choices. To get started you can choose to do some of the obvious things to improve your overall health, such as move more, drink less, quit smoking if you do smoke, decrease saturated fats in your diet. From here you can start to look into the information available around lifestyle and diet for overall health and relating to MS and start to make decisions of your own. Remember, MS affects each person in a unique way, your approach to manage your MS may be different from others and that’s okay.
Where to next?
If you’ve made it here it’s clear you want to be proactive in managing your condition, that deserves a pat on the back.
It’s easy to feel overwhelmed, angry, lost, and helpless but I want to help you get control of what you can control and live a life you’re happy with.
First thing is to find a good neurologist, if you’re not happy with the one you are seeing, shop around; they will be in your life for a long time moving forward as MS is a lifelong condition, if you’re not happy with them now it’s unlikely you ever will be, so find someone you’re happy with.
Solidify your support network – whether in person or online, you can search social media for hashtags like #livingwithms to find other people to connect to, you can join support groups on facebook, or reddit, or join MS specific networks. In person, reach out to those around you, if you are ready to talk about your diagnosis. Whether you disclose your condition is up to you, and even if you don’t want to tell people you can still make good connections with your friends, your family, and more broadly in the community.
Find out more information, stay up to date on therapies and get support through some of these alliances. I personally follow MS Canada on YouTube as they freely share research updates and conference proceedings allowing me to stay up to date on the newest information.
Other than that, keep your chin up. An MS diagnosis can be devastating, overwhelming, and definitely life-changing, but if you’ve come this far you’re willing to do something about it. There isn’t much we can control when it comes to this disease and how it will impact us, but there are things we can control on how we live our life and the enjoyment we get from it. We can become more than our MS, we can become more because of it. Join me on this journey, reach out, share your experiences, and together we can make the best of the position we’re in at every moment.